GENERAL MEDICINE E-LOG
SUPRIYA GAGIREDDY 42
Hi,I am supriya 5th sem medical student.This is an online elog book to discuss our patients de-identified health data shared after taking his/her/guardians signed informed consent.Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This E-log book reflects my patient centered online learning portfolia.
CASE
A 60 year old female , daily labourer by occupation, resident of juhugudem came to OPD with chief complaints of
Chief complaints
1.Yellowish discoloration of eyes since 25 days.
2. Generalised weakness since 25 days.
3.fever since 25days
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 20 days back and developed a fever associated with burning micturition and yellowish discoloration of eyes for which she came to our hospital and advised admission but attenders doesn't want to get admitted.
Then she used some herbal medication on every monday for 2 weeks(I.e.. She used medication for 2 times) during which she skipped antihypertensives and antidiabetics.
Then she was fine until yesterday night and slept having dinner. Then she wake up at 2:00 AM for urination but she has difficulty in passing urine and couldn't pass urine. So she slept again and woke up at 5:00 AM and started developing sweating and weakness.
HISTORY OF PAST ILLNESS
K/c/o hypertension and DM since 6 years and on irregular medication
No History of CAD, TB, asthma, epilepsy.
TREATMENT HISTORY
For diabetes and hypertension she was using medications since 6 years .
For HTN: Tab. AMLONG 5 mg PO/OD
For DM: Tab. METFORMIN 500mg.,Tab. GLIMIPIRIDE
PERSONAL HISTORY
Occupation : Daily laborer
Diet : mixed
Appetite: normal
Bowel habits: irregular
Micturition: Abnormal
Addictions: toddy drinker occasionally but stopped after diagnosed with HTN and DM
FAMILY HISTORY
No significant family history
GENERAL EXAMINATION
Patient is conscious,coherent and co operative well oriented with time and place .
Well nourished and built
VITALS
Temperature: 98 °F
Pulse rate: 84 per min
Respiratory rate: 18 per min
BP: 140/90
SpO2: 99%
GRBS: 54mg%
PHYSICAL EXAMINATION
Pallor : absent
Icterus : present
Cyanosis : absent
Clubbing of fingers / toes : absent
Lymphadenopathy : absent
Edema : absent
SYSTEMIC EXAMINATION
CVS
S1 and S2 heard
No murmurs
RESPIRATORY SYSTEM
Dyspnoea : no
No Wheezing
Postion of trachea: central
ABDOMEN
Shape of abdomen: obese
No free fluid
Liver and spleen are not palpable
Bowel sounds are normal
CNS
Conscious
Speech : Normal
No signs of neck stiffness
There is no sign of meningeal irritation
Glasgow scale 15/15
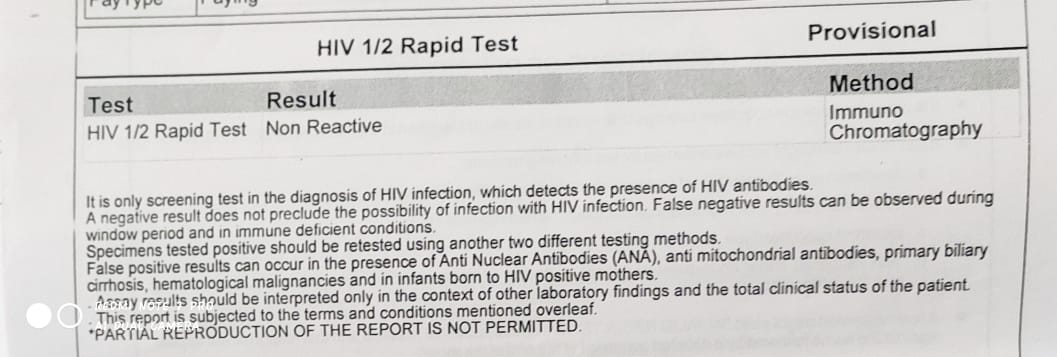
INVESTIGATIONS
On 01/07/2022
Complete Urine Examination
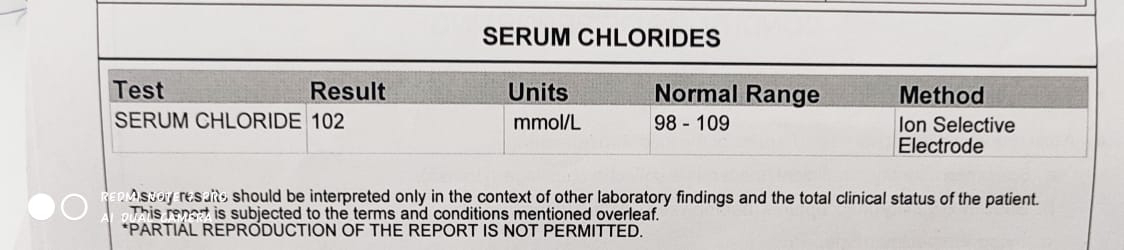
Serum Chloride
Ultrasound

PROVISIONAL DIAGNOSIS
?Viral Hepatitis
TREATMENT
On 18/07/2022
IVF-DNS 50ml
INJ- PANTOP 40 mg IV/OD
INJ. ZOFER 4 mg IV
TAB. UDILIV 300 mg PO/BD
Tab. WYSOLONE 10mg
Syp. LACTULOSE 25 ml PO
On 19/07/2022
INJ- PANTOP 40 mg IV/OD
INJ. ZOFER 4 mg IV
TAB. UDILIV 300 mg PO/BD
Tab. WYSOLONE 10mg
Syp. LACTULOSE 25 ml
INJ. NEOMOL 1gm IV/BDS
TAB. RIFAGUT 550 mg Po/BD
On 20/07/2022
INJ- PANTOP 40 mg IV/OD
INJ. ZOFER 4 mg IV
Syp. LACTULOSE 25 ml
INJ. NEOMOL 1gm IV/BDS
TAB. RIFAGUT 550 mg Po/BD
TAB. PCM 500 mg PO/BD
INJ. TRENEXA 500 mg IV/STAT
SYP. AROSTROZYME 25ml PO/TID













Comments
Post a Comment